Corneal Diseases and Surgery
Pacific Medical Centers has in-house, board-certified ophthalmologists. Among these specialists, we have a cornea and refractive surgeon. Our specialist has extensive training, which includes a fellowship focused solely on the diagnosis and treatment of corneal diseases and advanced refractive surgery techniques, including LASIK. This is in addition to the completion of a three-year ophthalmology residency approved by the Accreditation Council for Graduate Medical Education (ACGME). This level of training allows our specialist to diagnose and treat a broad range of eye conditions.
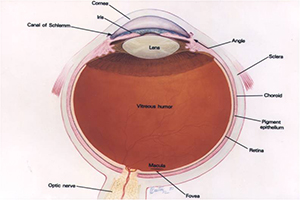
Ocular Anatomy
The cornea is the clear window of the eye. It is composed of five layers that work to maintain the cornea’s transparency, shape, and thickness to allow it to properly focus light as it enters the eye.
Some conditions and diseases that should be seen by a corneal specialist include:
Fuchs Endothelial Dystrophy
Fuchs Endothelial Dystrophy is an inherited disease that causes progressive swelling of the cornea and cloudy vision. As the eyes age, the defective corneal endothelial cells are unable to keep the cornea clear. Fortunately, a partial corneal transplant, called a Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK), can successfully replace the inner cornea layer with donor endothelial cells to restore function of the cornea.
Keratoconus
Keratoconus is a condition in which the cornea becomes progressively thinner. The abnormal corneal shape causes increasing astigmatism and near sightedness, and in severe cases, the cornea can become cone shaped. Some cases of keratoconus may stabilize, requiring only glasses or rigid gas permeable contact lenses. More severe cases may require cornea transplant procedures called a Penetrating Keratoplasty (PK) or Deep Anterior Lamellar Keratoplasty (DALK). Newer treatments of collagen crosslinking are currently undergoing research and may slow the progression of keratoconus in select cases.
Dry Eyes
Dry eye syndrome is one of the most common ocular conditions affecting patients. The normal tear film functions to create a smooth interface over the corneal surface to focus rays of light. A healthy tear film provides nutrients and oxygen to the cornea and protects against infections. With dry eyes, the tear film is unstable, causing symptoms ranging from mild irritation to constant foreign-body sensation and blurry vision. Certain drugs, medical conditions and increasing age cause a decrease in baseline tear film production. Blepharitis, which is a common inflammation of the eyelid’s oil glands, may also contribute to dry eye syndrome. These oil glands secrete an essential lipid layer to prevent rapid evaporation of the tears.
Treatment begins with using over-the-counter artificial tears. Thicker lubricating ointments or gels can be used before going to bed. Punctal plugs can occlude the tear drainage holes, helping to prolong the actions of tears. Prescription medications are sometimes indicated in severe dry eyes.
Corneal Infections
Bacterial and viral infections are common pathogens that may cause corneal ulcers. Herpes Simplex Virus is one of the most common recurrent infections of the cornea, often requiring long-term treatment. Varicella Zoster Virus, which causes shingles and chicken pox, may also infect the eye or eyelids. Adenoviral viruses are the cause of common pink eye infections; however, certain virus strains cause a more severe infection called epidemic keratoconjunctivitis.
Bacterial infections of the cornea are commonly due to poor contact lens hygiene or trauma. These can result in painful corneal ulcers and scarring, which require prompt treatment with proper antibiotic eye drops. In severe cases, a cornea transplantation may be needed.